Mental health conditions refer to a wide variety of conditions and disorders which effect mood, thinking and behavior. Mental health conditions are not always permanent, and as many as 1 in 5 Americans will have a diagnosable mental health condition in any given year.
Research has demonstrated the role of pet ownership and human-animal interaction (HAI) for improvements in mental health, including reduced anxiety, depression, and alleviating symptoms for those with Post Traumatic Stress Disorder (PTSD). The below provides an overview of the research findings on HAI for Stress, Anxiety, Depression, PTSD and Trauma.
For more information on HAI for mental health in children or older adults, please see:
Stress
Research indicates that pet ownership and HAI can positively impact stress through the reduction of stress-related parameters such as epinephrine and norepinephrine, improvement of immune system functioning, pain management, increased trustworthiness of and trust toward others, reduced aggression, enhanced empathy and improved learning.
The Effects of Pet Ownership on Stress
To measure the impact of companion animals on stress levels, many studies incorporate a transient stressor, such as having study participants perform a challenging arithmetic problem.
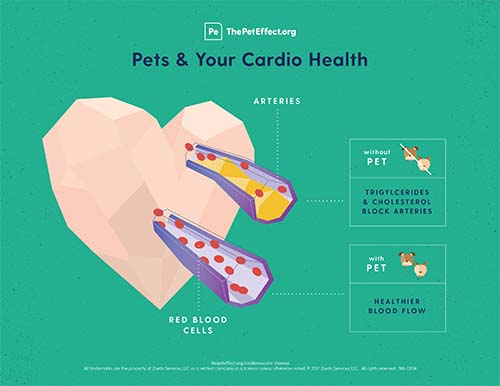
- One study examined the effect of pet ownership on cardiovascular responses to psychological stress (mental arithmetic task), comparing a group of hypertensive individuals in high-stress professions (stockbrokers) who owned pets to an identical, non-pet-owning group. On each study day, blood pressure and heart rate were recorded at baseline and after each mental stressor, which took the form of an arithmetic or speech test. All participants were treated with an ACE inhibitor, Lisinopril. The researchers hypothesized that the pet-owning group would exhibit reduced heart rate, blood pressure and renin responses to psychological stress. The study found that:
- Persons with low social support systems in particular are likely to experience health benefits from the enhanced environment that pets provide;
- ACE inhibitor therapy lowers only resting blood pressure, and the addition of a social support intervention lowers responses to stress.
- For the pet-owners in the study, the presence of pets provided the kind of non-evaluative social support that is critical to buffering psychological responses to stress.[1]
- Another study compared 45 adult female dog owners responses to stress after performing mental arithmetic tasks in laboratory and home settings.
- Results indicate that reactivity to a mental arithmetic task was moderated by the presence of a companion. Specifically, when compared with female subjects in a condition in which only the subject and a female researcher were present, female subjects in the condition in which their pet dogs were also present showed little or no physiological reactivity during performance of the stressful task, whereas female subjects in the condition in which their closest female friend was present showed substantially greater physiological reactivity.
- The researchers conclude that pet dogs provided the kind of nonevaluative social support critical to buffering physiological responses to acute stress.
- An exploratory study of stress-response behavior after interactions with a therapy dog found positive responses to both known and unknown therapy dogs on several physiological variables, such as blood pressure, heart rate, and salivary cortisol. The study compared the stress response of therapy dog owners interacting with their own therapy dog and people interacting with an unfamiliar therapy dog.
- The study results support a buffering effect on the stress response associated with owners interacting with their dogs that may extend to interactions with unfamiliar therapy dogs.
- While the therapy dog owners perceived less stress and anxiety after interacting with their familiar therapy dog, the unfamiliar therapy dog group experienced greater reductions in physiological measures such as blood pressure.
- In addition, positive attitudes toward pets was associated with decreased levels of self-reported stress, salivary cortisol, and SBP after interacting with the unfamiliar therapy dog.[2]
The Effects of Animal-Assisted Therapy (AAT) on Stress
Animal-assisted therapy has also been shown to reduce stress for university students.
- A study examining the impact of a 15-minute session between a therapy dog and a university student found that even in instances of limited sessions, interaction with a therapy dog can cause statistically significant reductions in perceived stress (state anxiety) and physiological markers of stress (blood pressure) in students.[3]
- A two-year, randomized controlled trial that examined the effects of animal-assisted therapy on stress levels of university students classified as being at high risk of academic failure.[4]
- Both immediately following interaction with a therapy dog and during a six-week follow-up, students expressed reduction in anxiety and an increase in confidence. After the six-week follow up, researchers also noted that students displayed increased problem-solving skills.
- Overall, the results provide evidence that interacting with therapy dogs and their handlers, either with or without exposure to formalized stress reduction content, improves behavioral aspects of academic success for university students who have been classified as being at high risk of academic failure.
For more information about stress:
Anxiety
Anxiety disorders are among the most common mental health conditions, encompassing a broad range of negative emotions including distress, fear, or uneasiness. A growing body of evidence suggests that the human-animal bond can reduce many symptoms of anxiety.
The Effects of Animal-Assisted Therapy for Anxiety
Many studies investigating the impact of pet ownership and human-animal interaction on anxiety focus on patients in clinical settings such as hospitals, who are prone to high levels of anxiety.
- In a study of hospitalized patients with heart failure, patients that received a therapy dog visit for 12 minutes had significantly greater decreases in systolic pulmonary artery pressure during and after and in pulmonary capillary wedge pressure during and after the intervention, compared to patients receiving usual care and patients who received visits from a human volunteer.
- Patients that received a dog therapy visit also had the greatest decrease from baseline in state anxiety sum score compared with the control groups.[5]
- A controlled clinical trial examined the impact of animal-assisted therapy on the anxiety levels of 93 patients in an emergency department of a hospital.
- Researchers found that after exposure to a therapy dog and its handler, anxiety levels were significantly reduced in the patients.
- In addition, while only one patient in the experiment group (receiving AAT) needed pain medication, compared to seven patients in the control group (received no therapy).[6]
- A pilot study conducted to evaluate the effect of dog-assisted therapy for individuals with a history of anxiety related to dental visits examined the impact of a therapy dog’s presence during routine dental cleaning. To test the hypothesis, the study included self-assessments of the level of anxiety perceived by the patient in previous experiences at the dentist and the current experience assisted by a therapy dog.
- The presence of the therapy dog was found to significantly decrease patients’ anxiety levels, in addition to lowering their blood pressure.[7]
Research also indicates that petting and observing companion animals can also play a role in reducing anxiety.
- In two separate experiments, participants of a mixed method models study were asked to watch identically equipped fish tanks for five minutes in each of three conditions: (1) live fish, (2) plants and water, and (3) empty tank.
- Results showed greater perceptions of relaxation and mood, and less anxiety during or after viewing the live fish condition, compared with the other conditions.
- Researchers conclude that likely explanations for this reduced stress include the fish providing a pleasant distraction, and a possible form of companionship.[8]
- Results of a study of 58 non-clinical individuals in a stressful situation demonstrated that a short period of petting an animal resulted in reduced state-anxiety.
- While the anxiety-reducing effect of the petting did not occur when petting toys in a control group, the effect of petting animals was not limited only to soft animals, and was also found to hold for hard-shelled animals like a turtle and, leading researchers to conclude that it was the quality of being alive rather than the texture of the object that produced the effect.[9]
For more information about anxiety:
Depression
Depression and depressive disorders are a category of mood disorders that involve extended periods of feeling extremely low that disrupt a person’s ability to enjoy life. Scientific research on the efficacy of the human-animal bond and human-animal interaction focus on the impact of animals on the ability to improve mood.
The Effects of Animal-Assisted Therapy for Depression
A growing body of literature suggests that AAT can be an effective, complementary treatment for reducing depression and improving mood.
- In one study of residents in a long-term care facility, after introducing residents to structured visits with a therapy dog for six weeks, those who visited the therapy dog reported significantly lower depression levels, as measured by the Beck Depression Inventory, compared to the control group. Results indicate that animal-assisted activities (AAA) can make a positive difference in the depression levels of residents in long-term care facilities.[10]
- In a study of 69 psychiatric inpatients, AAT led to a significant increase in interactions with other patients over the course of four weeks in comparison to rehabilitation without animals.
- Interactions included smiles, sociability, helpfulness toward others, activation and responsiveness.[11]
- Researchers conclude that AAT can enhance the existing benefits of conventional therapy.
- A study of the effects of AAT for 10 patients with chronic schizophrenia found that a 10-week AAT-program increased capacity for the patients to feel pleasure in comparison with a group without AAT.[12]
The Effects of Pet Ownership for Depression
- A study using data from 460 patients examined the relationship between the recovery process following a heart attack, depression, and pet ownership.
- Not only was pet ownership associated with decreased mortality after adjusting for the effects of depression, but also the effect of pet ownership tended to moderate the effect of depression on mortality.
- Pet ownership may be particularly beneficial for depressed post-MI patients in that it tended to enhance survival most in patients who remained depressed at least six months after their MI.[13]
For more information about depression:
Post-Traumatic Stress Disorder (PTSD)
PTSD is an anxiety disorder characterized by symptoms related to intrusion, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity. According to the U.S. Department of Veterans Affairs, PTSD affects more than 250,000 (30 percent) of post 9-11 war veterans, with an alarming 22 suicides per day.[14][15]
Animal-Assisted Interventions (AAI) for PTSD
A systematic literature review funded by HABRI and conducted by Dr. Marguerite O’Haire from Purdue University provides a comprehensive overview of empirical research on AAI for trauma. The study evaluated the characteristics, evidence and reported outcomes of AAI for trauma.
The review concludes that results have been predominantly positive, showing short-term improvements in depression, PTSD symptoms and anxiety, highlighting:
- Reductions in Depression:
- The most common finding among the reviewed studies was reduced depression following AAI;
- A study examining veterans and horse riding found long-term reduction in depression, with positive changes lasting 12 weeks after the intervention. Studies examining interactions with other animals found short term reduction in depression following AAI.
- Reduced PTSD symptom severity:
- In a review of 10 studies, all reported positive outcomes of AAI for individuals who have experienced trauma, including 5 studies which noted a reduction in symptoms for PTSD compared to pre-intervention.
- The researchers suggest that reductions in depression may be related to changes in the PTSD symptom of negative alterations in cognition and mood.
- Two studies that examined dissociation as a separate symptom of PTSD found significant decreases in dissociation following AAI;
- Additionally, the presence of an animal is purported to act as a comforting reminder that danger is no longer present and has been reported to elicit positive emotions and warmth.
- Animals have also been demonstrated as social facilitators that can connect people and reduce loneliness, which may assist individuals with PTSD to break out of isolation and connect to the humans around them.
- Reduced severity of symptoms may also be linked to the centering ability of animals to act as a positive external focus of attention.
- Reduction in Anxiety:
- Another common finding was reduced anxiety. Four studies in the review reported reduced anxiety following AAI.
- In a study of 80 women watching a traumatic video, women who watched the video with a dog present self-reported lower levels of anxiety compared to women who watched the video alone or with a stuffed dog.
- Anecdotal evidence links a reduction in arousal due to the comforting soft contact of stroking an animal, and to the secretion of oxytocin that occurs when in the presence of an animal.
More information about this study can be found here.
The Effects of Service Dogs on Veterans with PTSD
Results of a preliminary study funded by HABRI and conducted by Purdue University, titled “Preliminary efficacy of service dogs as a complementary treatment for posttraumatic stress disorder in military members and veterans”, shows a wide range of benefits for military members and veterans with PTSD.
The study compared 141 post-9/11 military members and veterans with PTSD split in two groups, one group paired with a trained service dog with usual care, and one group on the waitlist to receive a trained service dog with usual care.
Results indicate that the addition of trained service dogs to usual care reduced overall PTSD symptomology and severity, noting:
- Military members and veterans with a service dog experienced a decrease in overall PTSD symptomology, including reduced levels of depression, and improved quality of life, physiological wellbeing, life satisfaction, and resilience.
- Military members and veterans with service dogs reported lower absenteeism from work. compared to those on the waiting list to receive a service dog.
- Military members and veterans with service dogs reported increased social functioning, including decreased loneliness and improved feelings of companionship.
The participants with service dogs received the same level of usual care compared to those on a waitlist to receive a service dog, indicating that service dogs provided complemental treatment for participants, and did not replace usual care.- In fact, participants with service dogs reported an average of 20% improvement from usual care, despite the dosages remaining the same compared to the control group.
More information about this study can be found here.
Results from this research were also published in a related study, “The effect of a service dog on salivary cortisol awakening response in a military population with posttraumatic stress disorder (PTSD).”[16]
Saliva samples from military members with a service dog and those on a waitlist to receive a service dog were taken at various points in the morning after awakening. Results show:
- Participants with a service dog demonstrated lower levels of salivary cortisol, indicating decreased sleep disturbance, and increased wellbeing compared to individuals on a waiting list.
- Military members and veterans with a service dog also displayed lower levels of anger and anxiety compared to individuals without a service dog.
- In addition, participants with a service dog displayed less alcohol abuse compared to individuals on the waitlist.
For more information about PTSD:
Trauma
AAT has been widely studied for individuals who have experienced trauma, including physical abuse, sexual abuse and unspecified trauma. Animal-assisted therapy has also been found to aid in the recovery process in children and youth who have experienced trauma.[17]
According to a review of literature on animal-assisted therapy for trauma, animals provide emotional security, psychophysiological and affect regulation, neurological and other behavioral responses of humans to our social environment that facilitate the healing process.[18]

Service animals and therapy animals have been trained to support those with PTSD.Photo: Loving Thunder
The Effects of Animal-Assisted Therapy for Survivors of Trauma
Multiple studies have demonstrated the benefits of equine-facilitated psychotherapy for survivors of trauma.
- One study conducted semi-structured interviews and video-tapes of horse-rider interaction to describe the nature of the equine-human bond and its contribution to recovery from trauma.
- The equine-human bonds described by participants have parallels both with important elements of therapeutic alliances between professionals and clients and with the positive impact of relationship factors on client outcome. The study concluded that horse riding improved participants’ self-esteem, and facilitated the healing process through strong emotional bonds and an opportunity for therapeutic contact in the form of riding and petting.[19]
For more information about trauma: